The COVID-19 treatment trials that ‘learn as they go’
This article was first published on Pursuit. Read the original article.
Written by Dr Robert Mahar, University of Melbourne, Associate Professor Steven Tong, Royal Melbourne Hospital and Doherty Institute, and Dr David Price, University of Melbourne and Doherty Institute.
At the time of writing, there is no known effective treatment for COVID-19, a serious and highly contagious respiratory disease that has caused a global pandemic, mass hospitalisations, and sadly, many deaths.
Quickly finding an effective treatment is paramount, but comes with many challenges.

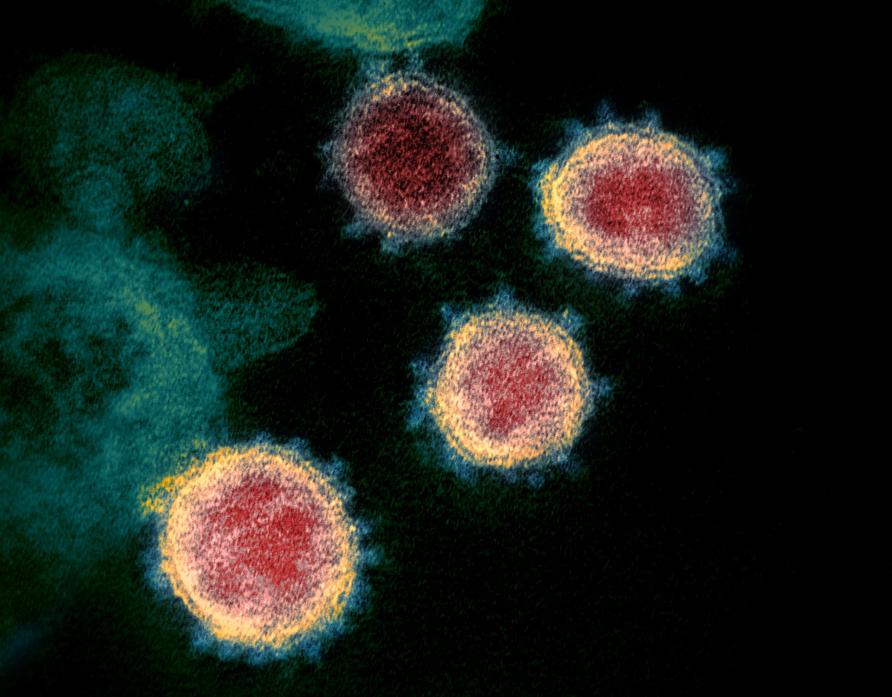
COVID-19 is caused by a novel coronavirus, named SARS-CoV-2, which was first detected in December 2019 in Wuhan, China. Being novel means the virus is completely new to science, so there is a limited understanding of how COVID-19 might best be treated and what the treatment outcomes might be.
But we have seen similar diseases this century that might hold some clues.
The novel coronavirus is similar to two other recently emerged coronaviruses: namely, severe acute respiratory syndrome (SARS-CoV), which first circulated in 2002-2003, and Middle East respiratory syndrome (MERS-CoV), which appeared in 2015.
Drugs that have been investigated as treatments for SARS or MERS include lopinavir and ritonavir, both used to treat human immunodeficiency virus (HIV) infection, and hydroxychloroquine, mainly used to treat arthritis or malaria.
The same drugs may be able to treat COVID-19 and have demonstrated some activity against SARS-CoV-2 in laboratory experiments, and in humans outside of the rigours of a clinical trial.
While lab experiments are a key step in assessing whether a drug has the potential to be an effective treatment, the real proof will come from rigorous studies in humans.
To date, there has been one commendable, yet ultimately small and inconclusive, human trial of lopinavir and ritonavir from Wuhan in early 2020, although several other human trials are now underway.
Challenges for COVID-19 trials
The traditional approach to discovering how a new treatment works when given to humans is to cycle through several, often lengthy, phases of clinical trials.
First, the study must assess safety of the proposed treatment (Phase 1) and then demonstrate that the new treatment is likely to be effective using a small number of people (Phase 2). Finally, it must confirm that the treatment is effective in a much larger number of people (Phase 3).
This process may take many years. Even then, it may fail to show that the new treatment is effective.
Fortunately, the safety of the candidate treatments that we have described is well-understood as they have already undergone these early trial phases for other diseases. But Phase 3 COVID-19 trials are now required to generate evidence to support effective treatment(s) of COVID-19.
Given the rapid spread and increase in detected case numbers across the globe, the challenge is to design trials so that we can identify effective treatments and start providing them to patients as quickly as possible. All in the face of uncertainty.
Meeting the challenges
Researchers at the Peter Doherty Institute for Infection and Immunity are leading a trial, currently underway, that steps up to the unique challenges posed by the current pandemic: the Australasian COVID-19 Trial, or ‘ASCOT’ for short.
The main aim of ASCOT is to assess whether lopinavir/ritonavir, hydroxychloroquine, or a combination of both treatments, will lead to improved outcomes for COVID-19 patients compared to the current standard of care.
In contrast to most traditional randomised trials, as ASCOT generates evidence for, or against, any particular treatment, the likelihood an individual is randomised to a particular treatment can be updated while the trial is underway.
This ensures that most patients entering the trial receive what appears to be an effective treatment, while still generating sufficient evidence to prove that the treatment is effective.
This unique aspect of ASCOT also means that we are able to stop the trial if one of the treatments gives us enough evidence that it will work, or drop any treatment that looks like it will not work before the trial would typically finish.
Further, as evidence is generated from other trials around the world about other promising treatments, we are able to seamlessly introduce these new treatments into our study.

The ASCOT study joins a growing cohort of trials that are taking a similarly ‘adaptive’ approach to finding effective COVID-19 treatments, including the WHO Solidarity, REMAP-CAP and RECOVERY trials.
Benefits of being Bayesian
The flexibility of ASCOT and similar trials to adapt is possible using Bayesian statistical methods, which allow evidence about treatments to be continually updated with new information as it becomes available, while at the same time maintaining trial integrity.
In other words, Bayesian methods allow trials to ‘learn as they go’.
The new information doesn’t have to be raw data, it could be expert opinion or results from other trials. This level of flexibility is difficult with classical, non-Bayesian approaches.
Bayesian statistical methods are useful in almost all medical research, but particularly so in clinical trials, where they can be used to design what are known as ‘Bayesian adaptive trials’.
Although classical statistical methods, like the ones many people learn in high school and university, can be used to design adaptive trials, the mechanics of the Bayesian approach allows information to be combined much more naturally and better resemble how we think in the real world.
A key strength of the Bayesian approach tends to be on the probability that a treatment works, rather than a less informative focus on what ‘works’ or ‘doesn’t work’ according to a statistical test.
Why be Bayesian in a pandemic?
In the event of an outbreak of an infectious disease, such as the current COVID-19 pandemic, we often know very little but are required to act very fast.
Designing a non-Bayesian trial to confirm whether a treatment works under uncertainty is difficult because the sample size and design features of the trial rely on assumptions about how the treatment will work.

The design cannot be modified easily, and so if those assumptions are ultimately incorrect, the trial may finish without providing any useful evidence about what treatments are effective.
An outcome like this in the midst of a rapidly evolving pandemic is, unfortunately, not unlikely. A key flaw of some early clinical studies of treatments for COVID-19 is that they were underpowered and did not provide sufficient evidence to inform treatment decisions.
If many people have the pandemic disease and it progresses quickly, a Bayesian adaptive trial can swiftly learn about existing treatments, abandon any that prove futile and expand to include new and promising candidates.
Facing a disease that in just over four months has resulted in more than 162,000 deaths reported globally as we write this, it goes without saying that these are crucial design features.
In a pandemic, as the medical community scrambles to learn more about the disease, using Bayesian adaptive trial designs can ensure that we quickly hone in on the most promising treatments.
In turn, an effective treatment may be found much sooner than otherwise possible which saves time, but most importantly, has the potential to save lives.
